Topics
03/03/2025
The Rise in Obesity is Closely Linked to the Consumption of Ultra-Processed Foods
Summary
(1) The NOVA classification system, developed in 2009 by a research group at the University of São Paulo, categorizes foods into four groups based on the degree and purpose of processing rather than type or their nutritional content.
【1】Unprocessed or minimally processed foods
【2】Processed culinary ingredients
【3】Processed foods (PFs)
【4】Ultra-processed foods (UPFs)
Ultra-processed foods (UPFs) are formulations made from multiple ingredients and undergo numerous industrial processes. They include sweet or savory snacks, confectioneries, instant foods, processed meat products such as sausages and ham, and most fast foods.
Increased UPF consumption is believed to be linked to rising rates of obesity and diet-related diseases.
(2) UPFs are high in refined carbohydrates, added sugars, salt, saturated fats, and trans fats, making them energy-dense. On the other hand, they are poor sources of fiber, protein, and micronutrients.
Additionally, they often contain flavorings, colorings, emulsifiers, preservatives, and other cosmetic additives.
(3) Since the 1980’s, UPF consumption has surged not only in developed countries but also in developing nations. UPFs now account for more than 50% of total daily energy intake on average in the U.S., U.K., and Canada.
(4) Several studies examining the relationship between UPF consumption and obesity have clearly shown that higher UPF intake is associated with an increased risk of obesity. In contrast, greater consumption of natural foods, such as vegetables, has been found to be inversely correlated with obesity.
(5) A U.S. research group found that individuals with high UPF consumption tend to eat fewer natural foods, such as fruits, vegetables, and fish, leading to a significant decline in overall diet quality.
(6) Processed food diets may result in lower diet-induced thermogenesis (DIT) compared to whole-food diets, potentially increasing net energy intake. Additionally, UPF diets may lead to overeating because they provide less satiety and make individuals feel hungrier than unprocessed food diets.
<My thought>
(7) Generally, UPFs are considered to promote obesity when consumed in excess due to their high energy density. However, I want to highlight the risk of “ultra-processing” itself. Since UPFs are low in nutrients and fiber, and are easily digested, if a diet is skewed toward refined carbohydrates and UPFs while lacking natural foods like vegetables, it can lead to intestinal starvation, potentially raising the body's set-point weight.
(8) It is not an overstatement to say that the sharp rise in being overweight, obesity, and many lifestyle-related diseases coincided with the rapid industrialization of food processing in the 1970’s and 80’s.
(9) The World Obesity Federation (WOF) warns that without policy changes and effective obesity prevention measures, more than half of the global population will be classified as obese or overweight by 2035. In my opinion, instead of focusing solely on “calories,” policies need to emphasize factors such as the degree of food processing, the number of chews, and the digestibility of food.
【 Full text 】
-
Contents
-
- Food classification by NOVA
- The Issues with Ultra-Processed Foods
- Consumption of UPFs and its association with obesity
- Impact of UPFs on overall diet
(1) Decrease in overall diet quality
(2) Increase in net energy intake
(3)Effects on ad libitum energy intake - Why do UPFs cause weight gain?
- Desired future measures
The endless diet wars among factions in various diets—such as low-carb, ketogenic, paleo, low-fat, and vegan—have caused substantial public confusion and fostered mistrust in nutritional science. However, it is not widely known that diverse diets recommendations often share a common piece of advice: to avoid ultra-processed foods[1].
Empirical evidence has shown that the rising obesity rates closely parallel the increased consumption of ultra-processed foods in many countries.
In this discussion, I’d like to explore the reasons behind this and, finally, mention how it relates to my intestinal starvation theory.
1. Food classification by NOVA
NOVA (not a acronym) is the food classification that categorizes foods based on the degree and purpose of food processing, rather than their nutritional content. It was developed in 2009 by a research group at the University of São Paulo in Brazil[2].
Conventional food classification systems categorize foods and ingredients based on their botanical origin or animal species, and nutrient composition.
As a result, whole grains are often grouped with breakfast cereals or cookies, and fresh chicken or pork are often classified alongside chicken nuggets or sausages.
When considering their their impact on health and disease, conventional food classifications no longer worked well[3].

NOVA classifies foods into four groups based on the nature, extent, and purpose of the industrial processing they undergo.
(1)Unprocessed or minimally processed foods
Fresh fruits and vegetables, and other natural foods (such as grains, milk, fish, and meat) that have undergone processes like removing inedible parts, drying, grinding, pasteurization, chilling, freezing, or vacuum-packaging.
(2)Processed culinary ingredients
Substances derived from Group 1 foods or from nature through processes that include pressing, refining, milling, or drying, such as oils, butter, sugar, and salt. These processed culinary ingredients are typically not consumed on their own.
(3)Processed foods (PFs)
These are typically made by adding Group 2 substances to Group 1 foods. Examples include canned vegetables, fruit in syrup, canned fish, cheese, and freshly made breads.
(4)Ultra-processed foods (UPFs)
These are formulations created by combining many ingredients and undergoing a sequence of industrial processes. Examples include breakfast cereals, soft drinks and fruit juices, sweet or savory snacks, confectioneries, instant foods, reconstituted meat products such as sausages and nuggets, and most fast food items[3,4].
2. The issues with ultra-processed foods
Food processing, in essence, refers to “various operations by which raw foodstuffs are made suitable for consumption, cooking, or storage,” and virtually all foods undergo some form of processing before being eaten. Therefore, processing itself is not inherently bad.
However, ultra-processed foods are not modified foods but formulations made mostly or entirely from substances derived from foods and additives through multiple industrial processes, with little to no Group 1 natural foods[3].
These foods are high in refined grains, added sugars, salt, saturated fats, and trans fats, making them energy-dense. On the other hand, they are poor sources of dietary fiber, protein, and micronutrients.
Additionally, flavorings, colorings, emulsifiers, non-sugar sweeteners, and other cosmetic additives are often added to these products to mask undesirable qualities of the final product[5].
Nevertheless, since the 1980s, the consumption of ultra-processed foods (UPFs) has rapidly increased not only in developed countries but also in developing nations, largely driven by transnational corporations.

UPFs are highly appealing because they are hyper-palatable and addictive, inexpensive, have a long shelf life, and can be consumed anytime, anywhere[3].
The evidence based on the NOVA classification so far suggests that the decline in minimally processed foods and home cooking, alongside the replacement of food supplies with ultra-processed foods, is associated with unhealthy nutritional profiles and an increase in several diet-related diseases[3].
3. Consumption of UPFs and its association with obesity
In studies on adults reporting the proportion of total daily energy intake from UPFs, the highest levels (on average) were reported in the USA (55.1–56.1%), followed by the UK (53–54.3%), Canada (45.1–51.9%), France (29.9–35.9%), Brazil (20–29.6%), Spain (24.4%), and Malaysia (23%)[6].
A cross-sectional study (2005–2014) on American adults, who were found to consume an average of 56.1% of their total energy intake from UPFs, revealed significant differences across quintiles. Those in the highest quintile (Note 1) consumed 84.5% of their total energy intake from UPFs, while those in the lowest quintile accounted for 25.4%[7].
(Note 1: Quintile refers to one of five equal measurements that a set of things can be divided into)
♦A cross-sectional time series study conducted in fifteen Latin American countries revealed that sales of UPFs were associated with changes in body weight in twelve of these countries from 2000 to 2009[8].
A cross-sectional study based on data from Brazil’s 2008–2009 Household Budget Survey found that household availability of UPFs was positively correlated with both the average BMI and obesity prevalence. Those in the highest quartile (Note 2) of household consumption of UPFs were 37% more likely to be obese compared to those in the lowest quartile[9].
(Note 2: Quartile refers to one of four equal measurements that a set of things can be divided into)
♦A study involving 6,143 participants from the UK National Diet and Nutrition Survey (2008–2016) classified foods recorded in four-day food diary according to the NOVA system. Consumption of UPFs was associated with increases in BMI, waist circumference, and obesity rates in both men and women. For every 10% increase in UPF consumption, the obesity rate increased by 18%.
Higher consumption of UPFs was observed among men, white British individuals, smokers, younger people, and those in lower social class groups[10].
♦A cross-sectional study involving 19,363 adults aged 18 and older from the 2004 Canadian Community Health Survey, found that individuals in the highest quintile of UPF consumption were 32% more likely to be obese compared to those in the lowest quintile. Higher UPF intake was associated with being male, younger age, lower educational attainment, physical inactivity, smoking, and being born in Canada[4].
♦A prospective cohort study conducted since 1999 among graduates of the University of Navarra in Spain tracked 8,451 participants who were not overweight at baseline for about nine years. Those in the highest quartile of UPF consumption had a 26% higher risk of developing overweight or obesity compared to those in the lowest quartile.
Moreover, on average, they consumed more fast food, fried foods, processed meats, and sugar-sweetened beverages, while, in contrast, their vegetable intake was the lowest. A higher consumption of UPFs was associated with lower adherence to the Mediterranean diet[11].
3. Impact of UPFs on overall diet
(1) Decrease in overall diet quality
♦A U.S. research group analyzed data on 5,919 children and 10,064 adults from the National Health and Nutrition Examination Survey (2015-2018) to investigate the relationship between UPF consumption and overall diet quality. Diet quality was assessed using the American Heart Association (AHA) diet score and Healthy Eating Index (HEI)-2015 score.
The estimated proportion of children with a poor diet gradually increased from 31.3 % in the lowest quintile of UPF consumption to 71.6 % in the highest quintile. Similarly, among adults, this proportion rose from 18.1 % in the lowest quintile to 59.7 % in the highest quintile.
As UPF intake increased, the consumption of healthy foods such as fruits, vegetables, nuts, and fish significantly decreased, while the intake of unhealthy foods such as refined grains, sugar-sweetened beverages, and added sugars increased.

The research group concluded that higher consumption of UPFs was associated with substantially lower diet quality among children and adults. These findings were consistent with previous studies conducted in several countries[12].
♦An Italian research group hypothesized that meal timing could also be linked to food processing and conducted a study to test this. They analyzed data on 8,688 individuals from the Italian Nutrition & Health Survey (INHES), conducted between 2010 and 2013. Subjects were classified as early or late eaters based on the population’s median timing for breakfast, lunch, and dinner.
Results showed that late eaters (breakfast after 7 AM, lunch after 1 PM, and dinner after 8 PM) were less likely to consume unprocessed or minimally processed foods compared to early eaters, while they consumed more processed foods (PFs) and UPFs. Late eating was also inversely associated with adherence to the Mediterranean diet[13].
The Mediterranean diet, which primarily consists of fruits, vegetables, legumes, nuts, olive oil, and fish, has been shown to be linked to reduced weight gain[14].
(2) Increase in net energy intake
A group of researchers in the U.S. conducted a crossover comparative study to ascertain the net energy intake of two different diets: one consisting of specific processed foods and the other of an isocaloric whole-food (WF) diet. Eighteen subjects consumed two types of sandwiches with the same calorie content but differing in processing levels.
The WF meal consisted of multigrain bread (containing whole sunflower seeds and whole-grain kernels) and cheddar cheese, while the PF meal consisted of white bread and a processed cheese product.
In this study, diet-induced thermogenesis (DIT)(Note 3) after consuming the PF meal was 46.8 % lower than that of the WF meal. The researchers concluded that this difference in DIT led to a 9.7 % increase in net energy-gain for the PF meal[15].
(Note 3) Diet induced thermogenesis (DIT) is the process by which the body increases its energy expenditure for several hours in response to food intake.
Regarding the significant reduction in diet-induced thermogenesis (DIT) observed with the PF meal, the researchers provided the following analysis:
Compared to whole foods, PFs are characterized by lower nutrient density (a lower content and diversity of nutrients per calorie), less dietary fiber, and an excess of simple carbohydrates. As a result, PFs are structurally and chemically simpler than whole foods, making them easier to digest[15,16].
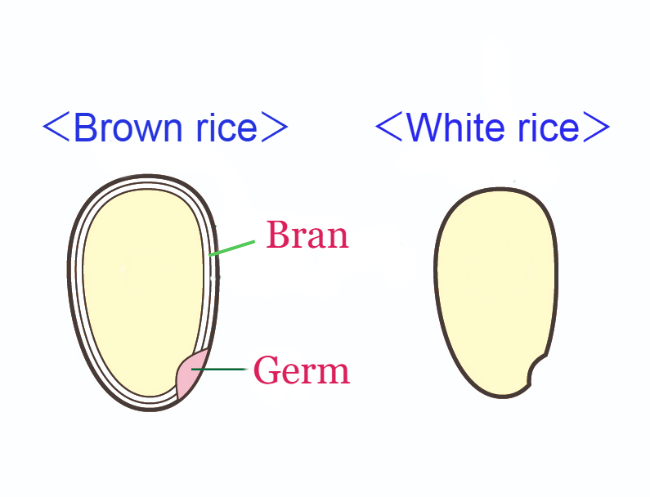
In grain refinement, most of the bran and germ are removed, resulting in the loss of nutrients (such as vitamins, minerals, and proteins), fiber, and phenols they provide.
Consequently, PFs tend to have fewer metabolites, leading to reduced enzyme production and peristalsis (Note 4), easier absorption, and less secondary metabolism—all of which contribute to lower DIT[15, 17].
Additionally, the loss of fiber reduces meal bulk and tends to slow satiety, both of which can lead to an increase in daily caloric intake[15, 18].
(Note 4:the repeated movements made by the muscle walls in the digestive tract tightening and then relaxing)
(3)Effects on ad libitum energy intake
A group of U.S. researchers conducted a randomized controlled trial to determine the effects of ultra-processed versus unprocessed diets on ad libitum energy intake in twenty adults with stable body weight. Subjects were randomly assigned to either the ultra-processed or calorie-matched unprocessed diet for two weeks, followed by the alternate diet for another two weeks.
In this experiment, participants were allowed to eat additional food after meals. As a result, they consumed more energy (459±105 kcal /day) during the ultra-processed diet and gained 0.4±0.1 kg of body fat. In contrast, they lost 0.3±0.1 kg of body fat during the unprocessed diet.
Fasting blood tests showed that levels of the appetite-suppressing hormone peptide YY (PYY) increased during the unprocessed diet as compared with both the ultra-processed diet and baseline. Also, levels of the hunger hormone ghrelin decreased during the unprocessed diet compared to baseline. This suggests that participants felt less hungry during the unprocessed diet, whereas the ultra-processed diet provided less satiety, making participants feel hungrier[19].
4. Why do UPFs cause weight gain?
I would like to explain the link between consumption of UPFs and an increase in obesity from the perspective of intestinal starvation.
Since the development of the NOVA classification, various studies have focused on the degree of food processing rather than calorie content, which is noteworthy.
In the past, factors such as refined carbohydrates, fast food, late-night eating, lack of vegetables, wealth, and poverty have been discussed as causes of being overweight. However, how these factors interact had not been clearly proven.
This time, research has shown that increased UPF consumption itself is linked to an overall decline in diet quality, lack of vegetables, late-night eating, and lower-income groups in developed countries.
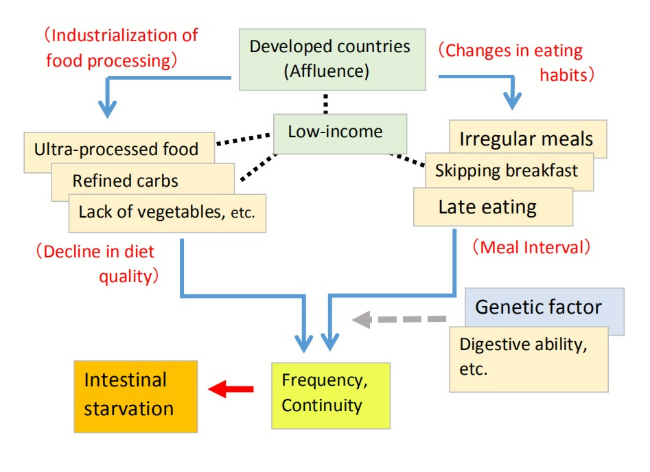
Through this blog, I have explained that a combination of factors—such as an unbalanced diet leaning toward refined carbohydrates and UPFs, a lack of vegetables, and an irregular lifestyle—can induce intestinal starvation, potentially raising the body's set-point weight.
UPFs are often high in energy density, so they are generally believed to promote obesity when overeaten. However, I believe the biggest issue is the "ultra-processing" itself, as these foods are digested and absorbed more quickly than natural foods.
If the diet is skewed toward refined carbohydrates and UPFs, and the overall diet quality declines, blood sugar levels can fluctuate sharply. Additionally, since these foods leave nothing behind in the intestines after digestion, intestinal starvation can be triggered (Note 5).
The fact that adherence to the Mediterranean diet and the consumption of natural foods like vegetables are inversely correlated with obesity supports my perspective.
In Japan, In my opinion, the consumption of UPFs such as instant foods, cookies, sweet bread, and chocolate confection is not necessarily low. However, one reason Japan’s obesity rate is lower than in Western countries may be its rice-based food culture, and the fact that many Japanese people still follow traditional eating habits.
(Note 5: Foods high in fat, such as ice cream, take longer to digest and may help prevent intestinal starvation.)
5. Desired future measures
The World Obesity Federation (WOF) warns that if policy directions remain unchanged and no effective measures are taken to prevent and treat obesity, more than half of the global population will be classified as overweight or obese by 2035.
I think this suggests that past policies focused solely on "calories in/ calories out" have not been particularly effective.
What we need now is a shift in focus from "calories" to factors such as the degree of food processing, the number of chews, and digestibility in policymaking.
With traditional dietary habits in many parts of the world, minimally processed natural foods were gradually digested in the digestive tract, allowing energy and nutrients to enter the bloodstream over several hours, while indigestible components like fiber helped maintain gut health.
Even if refined carbohydrates—such as white rice or bread—were included, the overall dietary quality likely remained high.
Even when people felt hungry, fiber and other undigested matter remained in the gut. As a result, there was little need to worry about caloric intake.

However, many people today prefer soft foods that require little chewing and have become overly reliant on refined carbohydrates and UPFs. These diets are low in nutrients and fiber, making them easy to digest, allowing the body to absorb large amounts of energy with minimal effort.
Moreover, once all the food is fully digested in the intestines, a signal that “there is no food” might be sent to the brain.
Such dietary habits were likely rare, if not nonexistent, in human history—at least until around 1970. It is not an overstatement to say that the sharp rise in being overweight, obesity, and many lifestyle-related diseases coincided with the rapid industrialization of food processing in the 1970’s and 80’s.
<References>
[1]Katz DL, Meller S. Can we say what diet is best for health? Annu Rev Public Health. 2014;35:83-103.
[2]Monteiro CA et al. NOVA. The star shines bright. Food classification. Public Health. World Nutr. J. 2016, 7, 28–38.
[3]Monteiro CA et al. The UN Decade of Nutrition, the NOVA food classification and the trouble with ultra-processing. Public Health Nutr. 2018 Jan;21(1):5-17.
[4]Nardocci M et al. Consumption of ultra-processed foods and obesity in Canada. Can J Public Health. 2019 Feb;110(1):4-14.
[5]Fiolet T et al. Consumption of ultra-processed foods and cancer risk: results from NutriNet-Santé prospective cohort. BMJ. 2018 Feb 14;360:k322.
[6]Elizabeth L et al. Ultra-Processed Foods and Health Outcomes: A Narrative Review. Nutrients. 2020 Jun 30;12(7):1955.
[7]Juul F et al. Ultra-processed food consumption and excess weight among US adults. Br J Nutr. 2018 Jul;120(1):90-100.
[8]Ultra-processed food and drink products in Latin America: trends, impact on obesity, policy implications. Pan American Health Organization, Washington (DC) (2013)
[9]Canella DS et al. Ultra-processed food products and obesity in Brazilian households (2008-2009). PLoS One. 2014 Mar 25;9(3):e92752.
[10]Rauber F et al. Ultra-processed food consumption and indicators of obesity in the United Kingdom population (2008-2016). PLoS One. 2020 May 1;15(5):e0232676.
[11]Mendonça RD et al. Ultraprocessed food consumption and risk of overweight and obesity: the University of Navarra Follow-Up (SUN) cohort study. Am J Clin Nutr. 2016 Nov;104(5):1433-1440.
[12]Liu J et al. Consumption of Ultraprocessed Foods and Diet Quality Among U.S. Children and Adults. Am J Prev Med. 2022 Feb;62(2):252-264.
[13]Bonaccio M et al. Association between Late-Eating Pattern and Higher Consumption of Ultra-Processed Food among Italian Adults: Findings from the INHES Study. Nutrients. 2023 Mar 20;15(6):1497.
[14]Beunza JJ et al. Adherence to the Mediterranean diet, long-term weight change, and incident overweight or obesity: the Seguimiento Universidad de Navarra (SUN) cohort. Am J Clin Nutr. 2010 Dec;92(6):1484-93.
[15]Barr SB, Wright JC. Postprandial energy expenditure in whole-food and processed-food meals: implications for daily energy expenditure. Food Nutr Res. 2010 Jul 2;54.
[16]Fereidoon Shahidi. Nutraceuticals and functional foods: Whole versus processed foods. Trends in Food Science & Technology, Volume 20, Issue 9, 2009, Pages 376-387.
[17]Secor SM. Specific dynamic action: a review of the postprandial metabolic response. J Comp Physiol B. 2009 Jan;179(1):1-56.
[18]Roberts SB. High-glycemic index foods, hunger, and obesity: is there a connection? Nutr Rev. 2000 Jun;58(6):163-9.
[19]Hall KD et al. Ultra-Processed Diets Cause Excess Calorie Intake and Weight Gain: An Inpatient Randomized Controlled Trial of Ad Libitum Food Intake. Cell Metab. 2019 Jul 2;30(1):67-77.e3.
10/14/2024
The Increasingly Important "Set-Point" Theory of Body Weight: What are the Environmental and Behavioral Factors?
Summary
■In 1953, Kennedy proposed that body fat storage is regulated. In 1982, nutritionists William Bennett and Joel Gurin expanded on Kennedy’s idea and developed the set-point theory. This may help explain the recurring failure of long-term dieting.
■When an individual loses weight, the body significantly reduces energy expenditure beyond what would be expected based on changes in body composition and the thermic effect of food. It also increases appetite through hormonal regulation, and alters food preferences to drive the body weight back toward a predetermined set-point range.
■Since obese individuals also exhibit these compensatory metabolic adjustments in response to dietary restriction, obesity may be considered a natural physiological state for some people.
■This body’s set-point is thought to be established early in life and remains relatively stable unless altered by specific life changes, such as marriage, childbirth, menopause, aging, or illness.
■As demonstrated in overfeeding experiments conducted in Vermont in the 1960’s, even weight gain from temporary overeating can trigger compensatory mechanisms that bring body weight back toward its set-point range.
■However, this set-point model of body weight does not explain the global rise in obesity since around 1970. Some researchers point out that while metabolic resistance to sustaining a reduced body weight is strong, its resistance to sustained fat gain may weaken over time with prolonged consumption of high-calorie foods.
< My thoughts >
■As some researchers have suggested, whether obesity as a chronic disease can be cured is depend on understanding how genetic and environmental factors interact to adjust the body's set-point weight.
■Since it is generally believed that a positive energy balance is necessary for weight gain, some researchers suggest that today’s environment of continuous high-calorie food intake may result in irreversible weight gain, which also suggests an increase in set-point weight, but I have a different view.
■There are two types of weight gain. Weight gain from temporary overeating is due to a positive energy balance, but this is usually short-term, and body weight is likely to return to its set-point.
On the other hand, I believe that long-term, irreversible weight gain, which suggests an increase in set-point weight, is more likely triggered by a negative energy balance or internal signals of “food scarcity,” similar to cases where weight increases even more after periods of starvation or dieting.
■Since 1970, one notable change in our living environment is what I call “intestinal starvation.” In many parts of the world before 1970, even if people went a whole day without eating until the next meal, there were likely still fibers and other undigested substances left in the intestines.
However, in today’s society, where easily digestible foods—such as refined carbohydrates, certain kinds of protein, and [ultra-]processed foods—are widely consumed, intestinal starvation can be induced in as little as 8 to 10 hours depending on how one eats. Through the gut-brain axis, this may send a signal to the brain indicating "there is no food."
※For an explanation of why intestinal starvation may lead to irreversible weight gain—suggesting an increase in body's set-point weight—please see Section 4.
【 Full text 】
-
Contents
-
- Advances in understanding “set-point” theory
- Problems with the set-point model
- Environmental and behavioral factors influencing weight set-point
- Why intestinal starvation increases one’s set-point weight
<How to prove my theory>
- Advances in understanding “set-point” theory
As I've explained in previous blog posts, I believe that each person has an individual “set-point” for their weight, and that understanding how this set-point increases is the key to addressing the issue of obesity.
This time, I would like to share my thoughts on recent advances in research regarding the set-point theory of body weight, as well as the environmental and behavioral factors that influence it.
1. Advances in understanding “set-point” theory
<Obesity and weight loss attempts>
♦A fat person who insists that a lean friend has consistently eaten more than the fat person does, may well be telling the truth.(*snip*)
The group of obese patients who are greatly in need of our understanding are those who keep to a calorie intake of perhaps 1000 kcal per day, yet lose less than one kg per week. There is no doubt whatsoever that such people exist, and can be studied in a metabolic ward under conditions where 'cheating' is virtually impossible without being detected. Usually these are middle-aged women who have been perhaps 40 kg overweight, and who have already lost about 20 kg. They are often depressed, hypothermic, and have a low metabolic rate. The nature of this metabolic adaptation to a low calorie diet is not known (as of 1973), but it is a phenomenon which has been known since before 1920. [1](J S Garrow, 1973)
♦For obese individuals, a certain amount of weight loss is possible through a range of treatments, but long-term sustainability of lost weight is much more challenging, and in most cases, the weight is regained [2]. In a meta-analysis of 29 long-term weight loss studies, more than half of the lost weight was regained within two years, and by five years, more than 80% of lost weight was regained [3,4].
In addition, studies of those who are successful at sustained weight loss indicate that the maintenance of a reduced degree of body fatness will probably require close attention to energy intake and expenditure, perhaps for life[5].
<Metabolic values of obese individuals>
♦The hypometabolic thesis had fallen out of favor by 1930, when more accurate calculations of body-surface area indicated that the metabolic rates of obese individuals were normal[6].
♦Total energy expenditure (TEE) in a day consists of three components: diet-induced thermogenesis (DIT), physical activity energy expenditure (PAEE), and resting energy expenditure (REE). When comparing a model case of men with an average weight of 100 kg and 70 kg, the man weighing 100 kg has a higher TEE[7] .
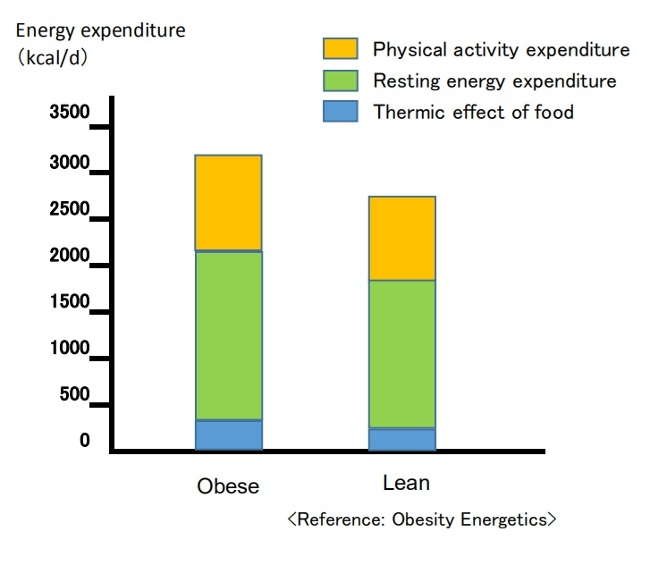
(Breakdown of energy expenditure in average 100-kg and 70-kg men)
Contrary to popular belief, people with obesity generally have a higher absolute REE compared to leaner subjects.This is because obesity increases both body fat and metabolically active fat-free mass[7,8].
PAEE can be subdivided into "voluntary exercise" and “activities of daily living.” Despite typically engaging in less physical activity, obese individuals often have a daily energy cost for physical activity similar to that of non-obese individuals since PAEE is proportional to body weight [7,9]. Additionally, due to a greater food intake, their DIT also tends to be higher [7].
<Dynamic changes in energy expenditure>
♦Obesity prevention is often erroneously described as a simple bookkeeping matter of balancing caloric intake and expenditure [10].
In this model, energy intake and expenditure are considered independent parameters determined solely by behavior. It is assumed that an obese person can steadily lose weight by eating less and/or moving more at a rate of one pound for every 3,500 kcal (or one kg for every 7,200 kcal) of accumulated dietary caloric deficit [7,11]. This view has been referred to as a “static model” of weight-loss, but it has been shown to be physiologically impossible [7,12].
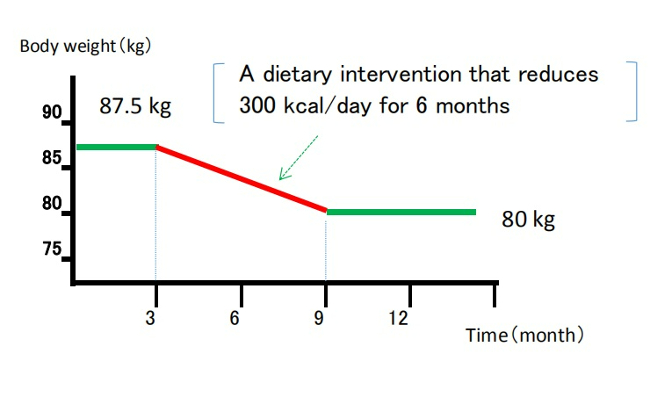
(Static model of weight loss)
(Despite being recognized as overly simplistic, the 3,500 kcal rule continues to appear in scientific literature and has been cited in over 35,000 educational weight-loss websites as of 2013.) [12,13]
♦It is now understood that energy intake and expenditure are interdependent variables, influenced by each other and by homeostatic signals triggered by changes in body weight [7,14].
Attempts to alter energy balance through diet or exercise are countered by physiological adaptations that resist weight loss [7].
<Set-point theory of body weight>
♦In recent years, the influence of homeostatic control has been recognized, and there is growing evidence that the body employs physiological mechanisms to manipulate energy balance and maintain body weight at a genetically and environmentally determined "set-point."[12]
In 1953, Kennedy proposed that body fat storage is regulated [15]. In 1982, nutritional researchers William Bennett and Joel Gurin expanded on Kennedy's concept when they developed the set-point theory [16]. The model has been widely adopted, and strengthened particularly after the discovery of leptin in the 1990’s [7,12].
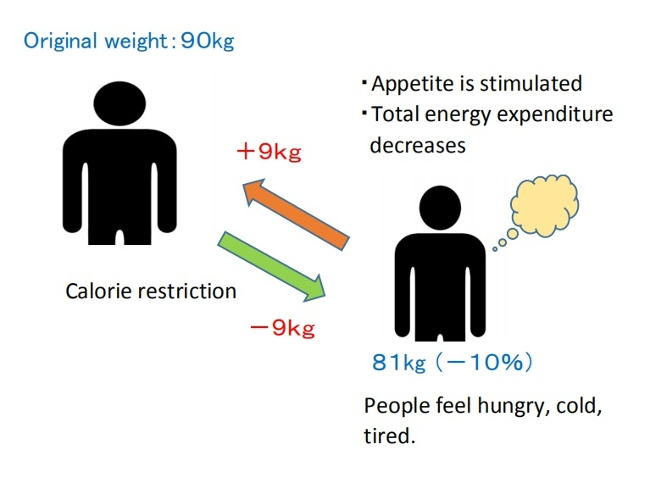
When an individual loses weight, the body significantly reduces energy expenditure to a degree that is often greater than predicted based on changes in body composition and the thermic effect of food. It also causes an increase in appetite through hormonal regulation and alters food preferences through behavioral changes, to drive the body weight back toward its set-point range[7,16].
( Set-point model of weight loss)
♦Weight-loss studies have shown that the magnitude of fat stores in the body is protected by mechanisms mediated by the central nervous system, which adjust energy intake (EI) and expenditure (EE) via signals from adipose tissue, the gastrointestinal tract, and endocrine tissue to maintain homeostasis, and resist weight change (set-point model)[12,17].
♦The body's protective metabolic mechanism that attempts to preserve energy stores during an energy crisis is known as adaptive thermogenesis (AT) or metabolic adaption[7,12].
AT is defined as the underfeeding-associated fall in resting energy expenditure (REE), independent of changes in body composition[12].
♦Maintenance of a 10% or greater reduction in body weight in lean or obese individuals is accompanied by about 20 to 25% decline in 24-hour energy expenditure. This reduction in weight maintenance calories is 10 to 15% lower than what is predicted based solely on alterations (/changes) in fat and lean mass [17,18].
Since obese individuals also display these compensatory metabolic adjustments in response to dietary restriction, obesity may be considered a natural physiological state for some people. Experimental studies on obesity in animals similarly suggest a view of obesity as a condition of body energy regulation at an elevated set-point [19].
♦A meta-analysis of cross-sectional studies investigating adaptive thermogenesis (AT) by comparing formerly obese subjects who had lost weight with BMI-matched subjects who were never obese, reported a 3–5 % lower resting energy expenditure (REE) in formerly obese subjects compared to never obese controls[20].
This effect means, for example, that if an obese woman reduced her weight from 100kg to 70kg, she would have to consume fewer calories to remain at 70kg than a woman who had consistently weighed 70kg[6]. Similar results have been confirmed in animal experiments involving obese and normal-weight rats.
This suggests that the frequent claim made by obese people that they eat the same or less than their lean friends but lose no weight, must be given more credence than it is ordinarily accorded[19].
♦On the other hand, as shown in overfeeding experiments on prisoners in Vermont in the 1960’s (Doctor Ethan Sims), weight gain due to temporary overeating also triggers compensatory mechanisms that bring body weight back into a set-point range.
However, some researchers point out that these may be weaker than those protecting weight loss. This asymmetry could be due to the evolutionary advantage of storing fat to survive during periods of caloric restriction, such as prolonged starvation [16,17].

♦In addition, hyperphagia (overeating) has been demonstrated following experimental semi-starvation and short-term underfeeding, which is probably the result of homeostatic signals resulting from the loss of both body fat and lean tissue [7,21].
♦This theory also suggests that a person's set-point for body weight is established early in life and remains relatively stable unless altered by specific conditions. However, the set-point may change throughout one’s life due to factors such as marriage, childbirth, menopause, aging, and disease [16].
On the other hand, the set-point theory remains a theory because all the molecular mechanisms involved in set-point regulation have not been elucidated, and some researchers may consider this theory to be overly simplistic[16].
2. Problems with the set-point model
However, some researchers have pointed out problems with the set-point model of regulation.
If such a powerful biological feedback system regulating the state of our body fat exists, then why do many individuals in most Western countries gain weight throughout majority of their lives? In particular, they argue that this model cannot explain the increasing prevalence of obesity that has been observed in many societies worldwide since the 1970’s[22].
In response, some researchers argue that while metabolic resistance to sustaining a reduced body weight is strong, metabolic resistance to sustained increased adiposity may not be physiologically long-lasting. The steadily increasing prevalence of obesity in humans also suggests that the state of body fat is facilitated more vigorously than losing weight[17,23].
Animal studies in mice demonstrated increased energy expenditure and increased sympathetic nervous system (SNS) tone during the first 3-4 weeks of consuming a high-fat diet, while these changes were no longer evident after a few months of high-fat diet consumption[17,24].
Another animal study in mice reported that long-term consumption of palatable, high-energy diets such as potato chips, cheese crackers, cookies, etc., caused irreversible weight gain, suggesting an increase in the set-point weight[19,25]. This effect is believed to be due to the increases in the number of fat cell[19,26].

■These explanations may sound reasonable at first, but in my opinion, this is no longer a "set-point" and it fails to explain why the body stubbornly shows metabolic resistance to maintaining weight loss, even at a higher set-point weight.
When applied to humans, not everyone who frequently consumes high-calorie foods becomes obese. This brings up several contradictions, such as:
(1)Why is obesity more prevalent among the lower-income groups in Western societies[22,27] and relatively wealthier groups in developing societies?[28];
(2)The coexistence of undernutrition and obesity in poor populations, observed globally since the 1950’s[29];
(3) Why do some people gain weight after environmental changes such as entering college, getting married, having children, or moving from Asia to Western countries?[22]
As I have mentioned repeatedly in this blog, I believe that an increase in set-point for body weight is due to inducing intestinal starvation, and that I can explain all these contradictions.
In the following section, I will explain that more specifically.
3. Environmental and behavioral factors influencing weight set-point
In 2012, the American Association of Clinical Endocrinology (AACE) designated obesity as a chronic disease. One of the rationale for that designation is that, like other chronic diseases, the pathophysiology of obesity is complex, involving interactions of genetic, biological, environmental, and behavioral factors[30].
Some researchers interested in the body weight set-point theory argue that understanding how genes and the environment interact to regulate the set-point is essential to determining whether obesity, as a chronic disease, can be cured. However, they struggle to explain the many significant environmental and social influences[22].
■ I also believe that the set-point of body weight changes due to the interaction between (1) genetic and biological factors, and (2) environmental and behavioral factors, but this time, I will mainly discuss (2) in this article.
When considering changes in living environment since the 1970’s, most researchers blame the rise in obesity on the increased availability of high-calorie foods and a decrease in physical activity as society became more affluent. In other words, they believe that a positive energy balance is necessary for weight gain.
However, paradoxically, the fact that the increasing prevalence of obesity coincides with an increase in weight-loss attempts[31] suggests that our understanding of energy balance may be flawed[12].
As suggested by overfeeding experiments, “temporary weight gain from overeating” and “irreversible weight gain occurring over many years ” are different. In my view, obesity as a chronic disease arises rather from signals of negative energy balance or "food scarcity" in the body, as in the cases where people gain more weight than before after starvation or dieting.
[Related article]
The Overfeeding Study Suggests That "Overeating" Is Not the Cause of Obesity
■Despite its impact on our bodies due to changes in our living environments since the 1970’s, "intestinal starvation" remains unrecognized.
Intestinal starvation refers to a state where everything consumed is fully digested throughout the entire intestinal tract, and it can occur in today's affluent developed countries, developing countries, or even among the poor. When there is little or no fiber and everything has been digested, our bodies perceive it as having "no food."
【Related Article】
The Body Perceive That It Is More Starved than in the Past
Perhaps in many parts of the world before 1970, even if people went a whole day without eating until their next meal, there were likely still undigested substances like fiber and tough plant cell walls left in their intestines. However, in today’s society, with its abundance of easily digestible, refined carbohydrates, processed foods, and fast food, intestinal starvation can occur in as little as eight to ten hours, depending on eating habits.
Intestinal starvation is more likely to occur with frequent consumption of easily digestible refined carbohydrates (bread, noodles, rice, etc.), industrially processed meat or fish products, fast food, and snacks, etc., combined with a lack of vegetables and long periods of prolonged hunger (such as skipping breakfast, late-night meals, or irregular eating habits).
【Related Article】
■In the animal experiments on rats described in section 2 above, it was reported that consuming a "high-energy diet" for 90 days led to irreversible weight gain, suggesting an increase in the set-point. However, the "fattening” diet used in this experiment (Rolls et al., 1980) primarily consisted of highly palatable items like potato chips, cheese crackers, and cookies sold in supermarkets. Those foods contained 47.5% industrially processed refined carbohydrates (fat: 42%, protein: 10.5%) on an energy basis[25]. Moreover, rats only eat when they’re hungry, and they are capable of eating the same food repeatedly.
In contrast, the “chow” fed to the control rats may have been made from ingredients like ground wheat, ground corn, soybean meal, and fish meal, etc. In other words, just as our diets from over fifty years ago, it likely contained a high amount of indigestible components, such as fiber and tough plant cell walls.
Therefore, I question the conclusion that highly palatable "high-energy diets" alone caused the irreversible weight gain.
4. Why intestinal starvation increases one’s set-point weight
Below, I will explain the mechanism by which the set- point for body weight increases due to the induction of intestinal starvation. While some of it involves speculation, it is based on events that have happened to me several times. You may not believe it, but at least for me, it is 100% accurate.
■Let's assume there is a man who has maintained a weight of 70 kg for many years. Even though his weight may fluctuate slightly during busy periods or after overeating, his weight revolves around 70 kg, so his set-point would be considered 70 kg.
When intestinal starvation occurs, a signal that 'there is no food' is transmitted from the intestines (or small intestine) to the brain.
As a result, the body tries to absorb more nutrients, causing microscopic substances attached to the villi (or microvilli) in the small intestine to detach (Figure 1), thereby increasing the surface area for absorption and raising the absolute absorption ability.
In other words, I believe that weight gain, at least to some extent, involves not only an increase in body fat but also lean tissue such as muscle.
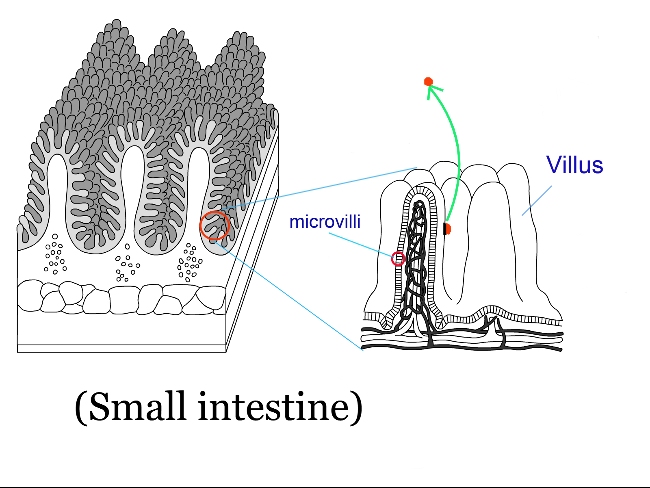
(Fig. 1 )
(Normally, a few undigested fiber or fats may remain, but when all food is perfectly digested, 5 to 10 kg of weight gain over a short period is possible.)
As a result, I believe the weight balancing point (the set-point) increases and reaches equilibrium within just a few days (Figure 2).
Weight gain does not occur from the gradual accumulation of excess calories each day, but rather in one sudden jump, possibly 0.3kg or 0.5g.
When dieting, the set-point can unknowingly rise, so you may gain a few pounds more than before once the diet ends.
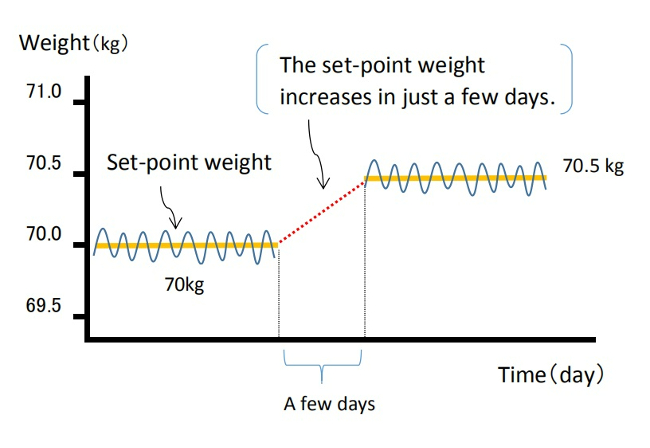
(Fig. 2 )
Once the body’s balance point rises, it becomes harder to lose weight because the overall absorption ability has increased. As mentioned in reference in section 1 , I agree with the idea that obesity is a “state of energy regulation at a higher set-point,” and is "a natural physiological condition" for obese individuals.
For more details, please refer to the article below.
【Related Article】
Gaining Weight by Intestinal Starvation; What Does It Mean?
<How to prove my theory>
It may be difficult to determine the exact cause when someone gains a few kg in a year, meaning their highest weight ever. However, I believe that, even with reduced calorie and carbohydrate intake from the meals I provide, it is possible to significantly increase a person's weight (by around 5 to 10 kg) within a few months, setting a new high set-point weight. By observing the data before and after, I think it is possible to investigate what changes have occurred inside the body.
<References>
[1]Garrow JS. Diet and obesity. Proc R Soc Med. 1973 Jul;66(7):642-4. PMID: 4741395; PMCID: PMC1645095.
[2]Wu T, Gao X, Chen M, van Dam RM. Long-term effectiveness of diet-plus-exercise interventions vs. diet-only interventions for weight loss: a meta-analysis. Obes Rev. 2009;10(3):313–323.
[3] Hall KD, Kahan S. Maintenance of Lost Weight and Long-Term Management of Obesity. Med Clin North Am. 2018 Jan;102(1):183-197.
[4]Anderson JW, Konz EC, Frederich RC, Wood CL. Long-term weight-loss maintenance: a meta-analysis of US studies. Am J Clin Nutr. 2001 Nov;74(5):579-84.
[5]Wing RR, Hill JO. Successful weight loss maintenance. Annu Rev Nutr. 2001;21:323-41.
[6]Jou C. The biology and genetics of obesity--a century of inquiries. N Engl J Med. 2014 May 15;370(20):1874-7.
[7]Hall KD, Guo J. Obesity Energetics: Body Weight Regulation and the Effects of Diet Composition. Gastroenterology. 2017 May;152(7):1718-1727.e3.
[8]Nelson KM, Weinsier RL, Long CL, et al. Prediction of resting energy expenditure from fat-free mass and fat mass. Am J Clin Nutr. 1992;56:848–856.
[9]Westerterp KR. Physical activity, food intake, and body weight regulation: insights from doubly labeled water studies. Nutr Rev. 2010;68:148–154.
[10] Levine DI. The curious history of the calorie in U.S. policy: a tradition of unfulfilled promises. Am J Prev Med. 2017;52:125–129.
[11] Hall KD, Chow CC. Why is the 3500 kcal per pound weight loss rule wrong? Int J Obes (Lond). 2013 Dec;37(12):1614.
[12] Egan AM, Collins AL. Dynamic changes in energy expenditure in response to underfeeding: a review. Proc Nutr Soc. 2022 May;81(2):199-212. doi: 10.1017/S0029665121003669. Epub 2021 Oct 4. PMID: 35103583.
[13]Thomas DM, Martin CK, Lettieri S et al. (2013) Can a weight loss of one pound a week be achieved with a 3500-kcal deficit? Commentary on a commonly accepted rule. In Int J Obes 37, 1611–1613.)
[14]Hall KD, Heymsfield SB, Kemnitz JW et al. Energy balance and its components: implications for body weight regulation. Am J Clin Nutr. 2012 Apr;95(4):989-94.
[15]KENNEDY GC. The role of depot fat in the hypothalamic control of food intake in the rat. Proc R Soc Lond B Biol Sci. 1953 Jan 15;140(901):578-96.
[16] Ganipisetti VM, Bollimunta P. Obesity and Set-Point Theory. 2023 Apr 25. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 37276312.
[17] Rosenbaum M, Leibel RL. Adaptive thermogenesis in humans. Int J Obes (Lond). 2010 Oct;34 Suppl 1(0 1):S47-55.
[18] Leibel R, Rosenbaum M, Hirsch J. Changes in energy expenditure resulting from altered body weight. N Eng J Med. 1995;332:621–28.
[19] Richard E. Keesey, Matt D. Hirvonen, Body Weight Set-Points: Determination and Adjustment, The Journal of Nutrition, Volume 127, Issue 9, 1997, Pages 1875S-1883S, ISSN 0022-3166.
[20]Astrup A, Gøtzsche PC, van de Werken K, et al. Meta-analysis of resting metabolic rate in formerly obese subjects. Am J Clin Nutr. 1999 Jun;69(6):1117-22.
[21] Dulloo AG, Jacquet J, Girardier L. Poststarvation hyperphagia and body fat overshooting in humans: a role for feedback signals from lean and fat tissues. Am J Clin Nutr. 1997;65:717–723.
[22]Speakman JR, Levitsky DA, Allison DB, et al. Set points, settling points and some alternative models: theoretical options to understand how genes and environments combine to regulate body adiposity. Dis Model Mech. 2011 Nov;4(6):733-45.
[23] Schwartz MW, Woods SC, Seeley RJ, et al. Is the energy homeostasis system inherently biased toward weight gain? Diabetes. 2003 Feb;52(2):232-8.
[24] Corbett SW, Stern JS, Keesey RE. Energy expenditure in rats with diet-induced obesity. Am J Clin Nutr. 1986 Aug;44(2):173-80.
[25] Rolls B.J., Rowe E.A., Turner R.C. Persistent obesity in rats following a period of consumption of a mixed high energy diet. J Physiol. 1980 Jan;298:415-27.
[26]Faust I.M., Johnson P.R., Stern J.S., Hirsch J. Diet-induced adipocyte number increase in adult rats: a new model of obesity. Am. J. Physiol., 235 (1978), pp. E279-E286
[27] Dykes J et al. Socioeconomic gradient in body size and obesity among women: the role of dietary restraint, disinhibition and hunger in the Whitehall II study. International Journal of Obesity 2004 Feb,:262-68.
[28] Poskitt EM. Countries in transition: underweight to obesity non-stop? Ann Trop Paediatr. 2009 Mar;29(1):1-11.
[29] Gary Taubes. 2011. Why we get fat. New York: Anchor Books, Pages 31-40.
[30]Garvey WT. Is Obesity or Adiposity-Based Chronic Disease Curable: The Set Point Theory, the Environment, and Second-Generation Medications. Endocr Pract. 2022 Feb;28(2):214-222.
[31]Montani JP, Schutz Y, Dulloo AG. Dieting and weight cycling as risk factors for cardiometabolic diseases: who is really at risk? Obes Rev. 2015 Feb;16 Suppl 1:7-18.
06/20/2024
The Overfeeding Experiment Suggests That "Overeating" Is Not the Cause of Obesity
Contents
- Can overfeeding experiments make people obese?
- Subsequent overfeeding experiments
- Can metabolism explain this weight regain?
- Difference between obesity and overfeeding experiments: My thoughts
1. Can overfeeding experiments make people obese?
According to George A. Bray (as of 2020, an emeritus professor at Pennington Biomedical Research Center), until the 1960’s, obesity was viewed as a "lack of will power," and many people thought, and some said "if only these patients would push themselves away from the table, they would not have this problem."
With this view of obesity, he reflects that the turning point for obesity being accepted as a bona fide area of academic interest were the studies on overfeeding. Overfeeding studies began to provide valuable insights into the biology of obesity. For Doctor Bray, who was a postdoctoral fellow at the New England Medical Center Hospital in Boston at the time, the excitement that was generated when the Vermont overfeeding studies were first presented in 1968 was unforgettable[1].
This was the case with the overfeeding experiments conducted by Doctor Ethan Sims in the late 1960’s. Until then, it was commonly believed that, "overeating obviously leads to obesity," so few such experiments had been conducted.
According to Dr. Jason Fung, the author of “The Obesity Code,” Dr. Sims recruited lean students at the nearby University of Vermont and encouraged them to eat a lot to gain weight. However, despite what both he and the students had expected, the students did not become obese.
Suspecting that the students might have been increasing their exercise, Dr. Sims changed course. He then recruited convicts at the Vermont State Prison as subjects. Physical activity was strictly controlled, and attendants were present at every meal to ensure the calories-4000 per day-were eaten.
Although the prisoners’ weight initially rose, it then stabilized. While some prisoners gained more than twenty percent of their original body weight, the extent of weight gain varied significantly among them[2] .

Over two hundred days on this overfeeding regimen, twenty inmates gained an average of twenty to twenty-five pounds. (About 10 kg.) However, once the experiment ended and their caloric intake returned to normal, the men had difficulty maintaining the weight gain, and most shed all the weight they had gained relatively easily. The exceptions were two inmates who struggled to lose that weight[3].
At the time, Dr. Bray was allowed to participate as a co-researcher in Dr. Sims' experiment to examine the metabolic changes occurring in adipose tissue during the weight gain that followed overfeeding.
Later, in 1972, he conducted his own overeating experiment, using himself as a guinea pig. Initially, he tried to double what he usually ate at each meal, but he couldn't finish, so he switched to energy-dense foods, such as ice cream.
Over the next ten weeks, he gradually gained ten kilograms, and repeated his tests such as measuring the thermic effect of foods.
But once he stopped stuffing himself, his weight rapidly decreased, returning to his original seventy-five kilograms six weeks later, and he has maintained this weight with no trouble ever since.
Following his self-experiment, the other four volunteers in this study began overeating in the summer of 1972. When the experiment ended, all the volunteers returned to their baseline weight.

Dr.Bray states that this rapid return to normal weight contrasts with the difficulties people with spontaneous obesity have in losing weight, and the even more difficult task of a maintaining a lower weight. Many who develop obesity over years suffer from a different kind of pain than those of us who acutely gain weight by overfeeding. For them, the obesity “slips up” on them and once present, is difficult to reverse.
The history of overfeeding and underfeeding trials and other lines of evidence clearly show that obesity prevention and treatment cannot simply rely on the advice to "eat less and exercise more." [1]
2. Subsequent overfeeding experiments
Alex Leaf (Western States University) and Jose Antonio (Nova Southeastern University) reviewed overfeeding studies conducted up to 2017 that evaluated various combinations of macronutrient overfeeding and its effects on body composition.
They found twenty-five overfeeding studies that reported changes in fat mass (FM) and fat-free mass (FFM), in addition to changes in body weight. The study durations ranged from nine to one hundred days, and all but four were conducted in sedentary populations[4]. Notably, the objectives of each study varied, and not all mentioned weight loss following the end of the experiments.
To give a few examples, a study on identical twins was published in 1990.
■Bouchard (Laval University, Canada) et. al. recruited twelve pairs of young adult male identical twins (twenty-four individuals) with no exercise habits. Each participant's energy requirements were measured during a two-week base-line period, and after that, they were overfed by 1000 kcal per day (comprising 15% protein, 35% fat, and 50% carbohydrates), six days per week, for a total of eighty-four days during a one hundred-day period. The men were housed in a closed section of a university dormitory, and were under supervision by staff all day.

The mean weight gain was 8.1 kg, of which 67% was fat mass (FM). However, the weight gain varied widely among participants, ranging from 4.3 to 13.3 kg[5].
Four months after the experiment ended, the twins' average weight was 61.7 kg, which was only 1.3 kg higher than their baseline weight of 60.4 kg, indicating they had almost returned to their original weight[1].
■Conford (University of Michigan) et. al. conducted a study in 2012 involving nine healthy, non-obese adults (seven men and two women). The participants were admitted to the hospital for two weeks, during which time they ate 4000 kcals per day (comprising 15% protein, 35% fat, and 50% carbohydrates). Their energy requirements were determined during a one-week baseline period before the start of the experiment. In addition to three main meals, they had four snacks each day. The average weight gain was 2.1 kg, of which 67 % was fat mass (FM).[6]
The summary of this review indicates that overfeeding healthy, sedentary adults with a diet moderately high in both carbohydrates and fats (35-50% energy intake each) and low in protein (11-15%) primarily results in a gain in fat mass (FM), which accounts for 60-70 % of the weight gain. Additionally, the increase in fat-free mass (FFM) may be due to an increase in body water content rather than skeletal muscle tissue. In contrast, diets with significantly increased protein intake showed favorable changes in body composition, even with increased energy intake[4].
3. Can metabolism explain this weight regain?
Why did the participant’s weight rapidly return to normal over the ensuing weeks when they stopped overeating?
According to Dr. Bray, one of the striking findings in this Vermont study was that to maintain the weight they gained after overfeeding, they required more energy per unit surface area than before weight gain. When Dr. Bray moved to the University of California in 1970, his new lab began operating to explore his hypothesis about why extra energy was required to maintain the increased weight[1].
■Leibel (Rockefeller University) et. al. conducted a study in 1995 involving eighteen obese (BMI of 28 or higher) subjects (Group A) and twenty-three subjects who had never been obese (Group B).
They measured changes in energy expenditure under three conditions: at their usual body weight, after losing more than 10 percent of their body weight by underfeeding, and after gaining 10 percent of their body weight by overfeeding.
When maintaining a body weight at a level 10% or more below their initial weight, the total energy expenditure decreased by 8±5 kcal per kilogram per day in Group A and by 6±3 kcal in Group B.
Conversely, when maintaining a body weight at a level 10% above their initial weight, total energy expenditure increased by 8±4 kcal in Group A and by 9±7 kcal in Group B.
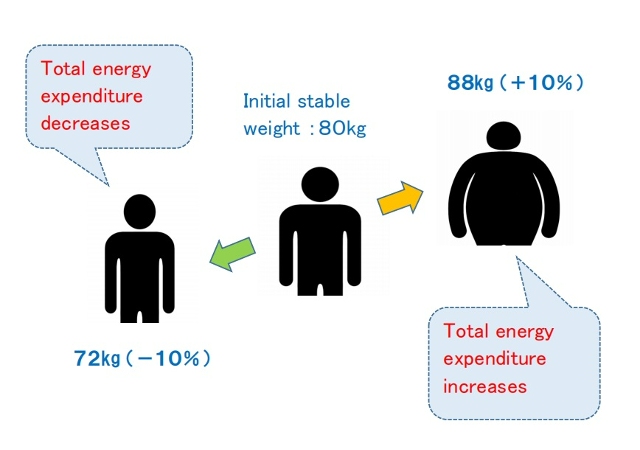
The study concluded that maintenance of a reduced weight or elevated body weight is associated with compensatory changes in energy expenditure, which resist maintaining the altered body weight and function to restore the original weight. This suggests that the long-term effectiveness of obesity treatment through caloric reduction may be limited[7].
4. Difference between obesity and overfeeding experiments: My thoughts
As Dr. Bray mentioned, I also believe that weight gain from temporary excessive caloric intake is due to body mechanisms entirely different from those underlying fundamental obesity. If compensatory metabolic mechanisms resist changes in body weight, why do some people continue to gain weight?
As I have repeatedly mentioned through this blog, the difference between people who are overweight and lean can be explained by the difference in set-point for body weight. (One's set-point weight goes up through intestinal starvation.)
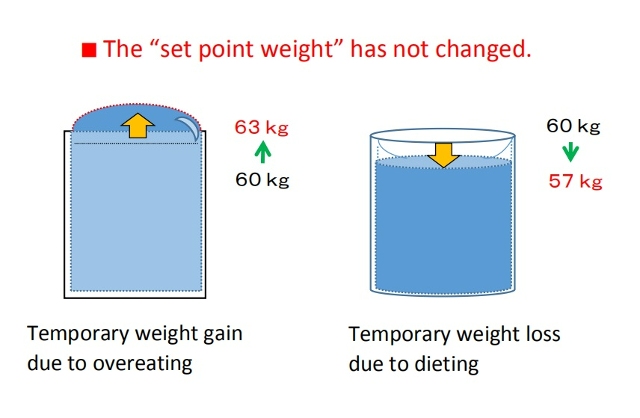
For example, suppose a person who normally weighs a stable sixty kg is temporarily overfed and reaches sixty-three kg.
This can be compared to a glass of water that is usually filled to about 97% now being filled to 100%, and then surface tension causing the water to rise above the rim.
Conversely, maintaining a weight of fifty-six kg by eating less is like the water level temporarily decreasing, causing a dip in the surface of the water.
In both cases, the set-point weight has not changed.
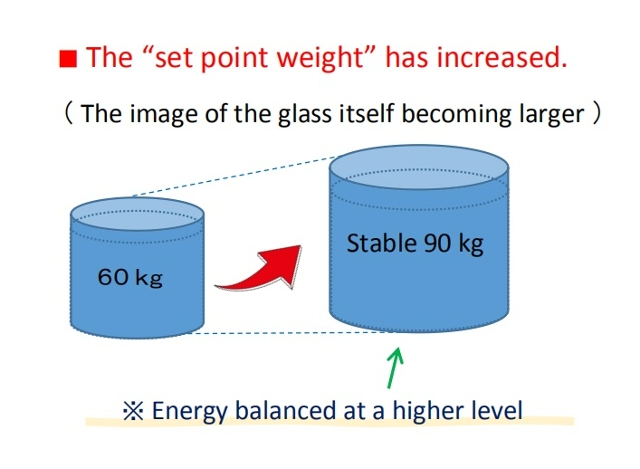
In contrast, if a person who originally weighs sixty kg gradually gains weight over several years, and then maintains a stable weight of ninety kg, this indicates that the set-point weight itself has increased, meaning the glass has grown larger, with energy balancing at a higher level.
Today, we are sometimes said to be living in an "obesogenic environment" that promotes obesity, but that does not necessarily mean consuming high-calorie foods or living sedentary lifestyles. As some researchers have already mentioned, calorie counting is clearly of little significance. Changes in caloric intake only lead to temporary weight gain or loss.
Rader, the "obesogenic environment" in my opinion is related to foods that are overly digestible foods (refined carbohydrates, fast food, processed foods, etc.) and an imbalanced diet (lack of vegetables, etc.). When these factors overlap with some other conditions such as skipping breakfast or eating late dinners, intestinal starvation is more likely to be induced.
Of course, researchers will say that in order to gain weight, more energy must be taken into the body than before. For more on why intestinal starvation leads to greater energy intake and weight gain, please refer to the article below.
[Related article] Gaining Weight by Intestinal Starvation; What Does It Mean?
<References>
[1]Bray GA. The pain of weight gain: self-experimentation with overfeeding. Am J Clin Nutr. 2020 Jan 1;111(1):17-20.
[2] Fung J, The Obesity Code, Greystone books, 2016, P114-116.
[3] Jou C. The biology and genetics of obesity--a century of inquiries. N Engl J Med. 2014 May 15;370(20):1874-7.
[4] Leaf A, Antonio J. The Effects of Overfeeding on Body Composition: The Role of Macronutrient Composition. Int J Exerc Sci. 2017 Dec 1;10(8):1275-1296.
[5] Bouchard C et al. The response to long-term overfeeding in identical twins. N Engl J Med. 1990 May 24;322(21):1477-82.
[6] Cornford AS et al. Rapid development of systemic insulin resistance with overeating is not accompanied by robust changes in skeletal muscle glucose and lipid metabolism. Appl Physiol Nutr Metab. 2013 May;38(5):512-9.
[7] Leibel RL et al. Changes in energy expenditure resulting from altered body weight. N Engl J Med. 1995 Mar 9;332(10):621-8.
02/08/2024
Diabetes (Dysglycemia) is Increasing Despite Decreased Carbohydrate Intake
Contents
- Trends in carbohydrate, fat, and energy intake in Japan(1955-2019)
- Background of the increase in dysglycemia in my opinion
<The bottom line>
If you haven't read the following article yet, please click here to read the original article.
A Low-Carb Diet in Japan:Reducing Carbohydrates Alone is Not the Only Crucial Factor
In this article, I will discuss the causes and background of the relationship between carbohydrate (sugar) intake and the risk of developing diabetes, dysglycemia, etc. in my own way. (The issue of obesity is not discussed in this article.)
1. Trends in carbohydrate, fat, and energy intake in Japan(1955-2019)
First, based on the National Health and Nutrition Survey conducted by the Ministry of Health, Labour and Welfare, the daily intake of carbohydrates, fat, and calories among the Japanese are shown below.
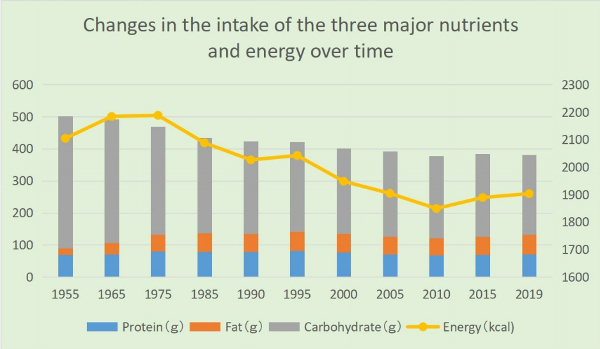
・Carbohydrate intake was 411g in postwar 1955, accounting for 78.1% of total energy intake, but it has been declining since then, reaching 280g in 1995 and 248g (52.1% of total energy intake) in 2019.
・As the economy developed in the postwar period, fat intake sharply increased to 50.1g in 1972 but has remained relatively stable around 55g since 1975. Although there was a slight decrease around the year 2000, annual variations after 1975 are not significant.
・Daily energy intake also increased from 2104 kcal in 1955 to 2287 kcal in 1971. However, there has been a decreasing trend since then, reaching 1903 kcal in 2019.
Nevertheless, the number of diabetes patients and those with blood sugar abnormalities continues to rise. The estimated number of diabetes patients (including those strongly suspected of having diabetes [*1]) has been steadily increasing since the survey began in 1997, from 6.9 million to 10 million in 2016.
If pre-diabetics [*2] with abnormal blood sugar are included, the number surpassed 20 million in 2016 (approximately one in six people). (From the 2016 "National Health and Nutrition Survey" in Japan).
[*1] Individuals with an HbA1c level of 6.5% or higher are considered to be "strongly suspected of having diabetes."
[*2] Individuals with an HbA1c level of 6.0% or higher but less than 6.5% are determined to have a "latent diabetes.”
2. Background of the increase in dysglycemia in my opinion
As evident from the above data, the increase in diabetes patients and individuals with blood sugar abnormalities in Japan cannot be solely explained by carbohydrate or caloric intake.
According to Dr. Yamada, the advocate of the low-carb diet, Japanese people have a weaker ability to secrete insulin than Westerners, and many people can have abnormal blood sugar level even if they are not overweight, but other factors I consider are as follows.
(1) Decline in physical activity
As many experts have pointed out, the increase in diabetes patients and those with blood sugar abnormalities is thought to be partially attributed to a decline in physical activity due to the widespread use of PCs, smartphones, video games, etc. (As for obesity, my theory is that decreased physical activity is not directly related to weight gain or obesity.)
(2) Statistical issues
■The National Health and Nutrition Survey selects about 6,000 households by stratified random sampling from designated unit areas. However, in the 2019 survey, it was reported that cooperative households amounted to 2,836, with 5,900 individuals. Since participation is voluntary, there is a tendency for less cooperation among groups such as men, young people, and singles[1].
■There may be a large gap between the upper and lower limits hidden in the averages. While some people follow an ideally balanced diet, others exhibit poor eating habits. In terms of carbohydrate intake, while some people eat fewer carbs due to dieting, people at high risk of lifestyle-related diseases may be consuming excessive amounts of carbs or have an unbalanced diet that leans toward instant foods, fast foods,etc.
(3) Meal frequency, timing, and more

Not only the quantity and quality of meals but also the frequency, timing, and order of consumption can impact absorption.
Skipping breakfast and having only two meals a day, even with the same amount of carbs at lunch, is said to increase absorption rates, causing a rapid rise in blood sugar levels after lunch.
In contrast, if you consume foods rich in dietary fiber,etc. at breakfast, it can have an impact on the post-lunch and subsequent meal (second meal) blood sugar elevation. This is known as the "second meal effect," as introduced by Dr. Jenkins from the University of Toronto, in 1982.
(4)Dietary balance
■Maintaining a balanced diet is important. Combining carbohydrates with other food groups such as meat, fish, oils, dairy products, and vegetables (fiber) will prolong gastric retention and moderate sugar absorption. This combination may help in controlling the rapid spike in blood sugar levels even with the same amount of carbohydrates. The tendency of many people to reduce fat intake in order to avoid gaining weight may lead to an increase in individuals with abnormal blood glucose levels as well as obesity.
■Since the 1970s, the rise of nationwide fast-food chains and franchise outlets in the food industry has increased opportunities for quick, convenient meals (such as beef bowls, curry, ramen, and hamburgers). These meals often lack vegetables and consist mainly of carbohydrates, potentially leading to a higher risk of blood sugar spikes.

In addition, many Japanese like to eat carbohydrates. Many set menus combine different types of carbohydrates (rice and wheat products), such as ramen noodles and fried rice.
Even if the amount of carbohydrates is small, combinations such as a rice ball and a snack bread (or instant noodles) can easily raise blood glucose levels.
(5) Quality of carbohydrates
■According to statistics from the Ministry of Agriculture in Japan, the per capita annual consumption of rice peaked at 118 kg in 1962 and has since been on a declining trend. By 2020, the consumption had decreased to less than half, reaching 50.8 kg. In addition, examining trends in annual expenditures per household, the amount spent on bread has exceeded the amount spent on rice since 2014.
While the consumption of rice has sharply decreased in recent years, it's crucial to note that there has likely been an increase in the intake of other carbohydrates that raise blood sugar levels, such as bread, sweets, candies, and soft drinks. Thus, relying solely on data related to “carbohydrate intake” may not provide a comprehensive understanding of the situation. (Reference: Japan Low-Carbohydrate Diet Study Group)

■In this context, the glycemic index (GI), which is quantified by blood glucose level and duration after ingesting a food containing 50 g of carbohydrate, is useful.
In addition, there is another indicator called Glycemic Load (GL), which is calculated by multiplying the percentage of carbohydrates in the target food by the GI value.
From the perspective of suppressing a rapid increase in postprandial blood sugar levels, it is important to focus on foods with a low GI/GL value(*3).
While foods such as white bread, refined rice, boiled potatoes, waffles, and french fries,etc are considered to have high GI values, it is worth noting that, foods like unpolished rice, wholegrain bread, beans, and nuts,etc. have low GI values.
(*3) It is said that foods that cause a rapid surge in blood sugar levels, like sugar, but quickly drop, cannot be adequately represented by the GI value.
■It is known that some starches in food, referred to as “resistant starch,” reach the large intestine without being digested. For instance, some starches found in rice, potatoes, and pasta, after being heated and gelatinized, undergo a structural change when cooled, with a portion turning into resistant starch.
Until around the 1970’s to 1980’s when insulated jars were not as common as they are today, it's likely that many people consumed even more resistant starch from "cooled rice" than they do now.
■In the late 1990’s, the National Cancer Center in Japan conducted a five-year follow-up study to investigate the association between carbohydrate intake and the incidence of typeⅡdiabetes. The study targeted approximately 65,000 men and women aged 45 to 75 with no history of diabetes, cardiovascular diseases, or cancer.
According to the findings, in women, there was a higher incidence of diabetes among those with higher intake of simple carbohydrates (sugar, fructose, etc.) and starches[2].
(6)Evolution of cooking, processed foods, etc
■In recent years, advancements in cooking techniques and the proliferation of processed foods have led to a softening of all types of food, including meat, fish, and vegetables, making them melt in the mouth. In my opinion, such foods, being quickly digested with reduced gastric retention time, may potentially accelerate the absorption of carbohydrates.
■Additionally, many processed foods and sweets often utilize artificial sweeteners. While these sweeteners themselves do not raise blood sugar levels, some experts suggest that their habitual use may impact glycometabolism through changes in taste preferences and alterations in gut microbiota [3][4].
The bottom line
(1) In Japan, since the 1955 statistics, carbohydrate intake has consistently decreased. Caloric intake has also been decreasing over the past fifty years. At least in Japan, the recent increase in diabetes patients and those with blood sugar abnormalities is not solely attributed to carbohydrate or caloric intake.
(2) When it comes to carbohydrates, the way blood sugar levels rise varies. The rapid westernization of the Japanese diet since around 1970 has resulted in a drop in rice consumption in Japan to less than half of its peak level in 1962. Instead, it is thought that the intake of processed wheat products (such as bread, noodles, and snacks) and sugar (sweets and soft drinks), which easily raise blood glucose levels, has increased.
Rice is a grain, and therefore the digestive process should be relatively slower compared to flour-based products, etc. However, even the same type of rice can raise blood glucose levels differently depending on the degree of milling, the cooking method, and the cooling method.
(3) I believe that how blood glucose levels rise is also heavily influenced by dietary balance, the frequency and timing of meals, order of intake, and other dietary habits.
For instance, I suspect that a diet that leans towards easily digestible carbohydrates, frequent intake of sugar, and eating habits such as skipping breakfast or fast eating can increase the frequency of insulin secretion, cause sharp fluctuations in blood sugar levels, and place a burden on the pancreas, even if the carbohydrate intake is not that high.
(4) In order to lower the risk of glucose abnormalities, isn't it important to be aware of not only the carbohydrate content of foods, but also how blood sugar levels rise, such as indicated by the Glycemic Index (GI) and Glycemic Load (GL)?
Reducing the intake of high-GI foods and sugars, and opting for low-GI foods (whole grains, protein-rich foods like meat and fish, nuts, dairy), oils, and non-starchy vegetables, is crucial to reduce overall dietary blood sugar elevation.
It's also known that eating regularly three times a day, starting with vegetables, and consuming cooled rice (resistant starch) can contribute to a gentler increase in blood sugar levels throughout the day.
(5) My personal opinion is that a traditional, well-balanced Japanese diet, with rice as the staple, is less likely to increase the risk of obesity and blood sugar abnormalities. Despite the fact that Japan is blessed with seasonal vegetables, seafood, and traditional fermented foods, I feel that in recent years more and more people are eating high GI carbohydrates, meat products, and instant foods, etc.
(For a comprehensive understanding of the effects of low-carb diets, including their impact on obesity causes, please refer to the following article.)
[Related article] A Low-Carb Diet in Japan:Reducing Carbohydrates Alone is Not the Only Crucial Factor
<References>
[1] Japan Society For The Study Of Obesity. Guidelines for the Management of Obesity Disease 2022. Life Science Publishing Co, Dec.2022, Page28.
[2] Kanehara R et al. Association between sugar and starch intakes and type 2 diabetes risk in middle-aged adults in a prospective cohort study. Eur J Clin Nutr. 2022 May;76(5):746-755. doi: 10.1038/s41430-021-01005-1. Epub 2021 Sep 20. PMID: 34545214.
[3] Pepino MY, Bourne C. Non-nutritive sweeteners, energy balance, and glucose homeostasis. Curr Opin Clin Nutr Metab Care. 2011 Jul;14(4):391-5. doi: 10.1097/MCO.0b013e3283468e7e. PMID: 21505330; PMCID: PMC3319034.
[4] Suez, J., Korem, T., Zeevi, D. et al. Artificial sweeteners induce glucose intolerance by altering the gut microbiota. Nature 514, 181–186 (2014). https://doi.org/10.1038/nature13793
02/07/2024
A Low-Carb Diet in Japan:Reducing Carbohydrates Alone Is Not the Only Crucial Factor
Contents
<Introduction>
- What’s Locabo?
- Summary of the effects of “Locabo"
- The increasing prevalence of diabetes in Japan
- Is controlling insulin the key to weight loss?
- The widespread issue of unbalanced and low-quality diets in Japan
<The bottom line>
<Introduction>
In Japan, since around 2015, the low-carb diet-we call "Locabo" based on the English term "a low-carb"-has been catching on among many people. Japan is traditionally a rice-eating culture, but after World War II, more and more people preferred bread and noodles, and with increasingly westernized diets, many feel that we are gaining weight as well.
This time, I’d like to introduce the Locabo diet in Japan, which is believed to be effective not only for losing weight but also for lowering abnormal blood sugar levels and other lifestyle diseases.
<My stance: I will approach the issues of obesity and blood sugar abnormalities separately.>
Generally, experts advocating for carbohydrate restriction seem to believe that the cause of obesity lies not in excessive caloric intake but in carbohydrates (sugars) that elevate blood sugar levels and stimulate insulin (*1) secretion (the carbohydrate-insulin model).
Additionally, it is believed that prolonged insulin resistance or decreased insulin secretion capacity, can lead to abnormal glucose metabolism, ultimately resulting in the development of lifestyle-related diseases such as diabetes.
In other words, both obesity and symptoms like blood sugar abnormalities are thought to be part of a series of events centered around insulin. However, I believe that obesity is caused by different mechanisms related to carbohydrates, so I would like to explain them separately.
(*1) Insulin is a hormone that lowers the level of glucose in the blood. It's released into the blood by the pancreas when the glucose level goes up. Insulin helps glucose enter the body's cells, where it can be used for energy or stored for future use.
1.What’s Locabo?
"In Japan, the phrase “carbohydrate restriction diet” has been generally used, but the word “restriction” has a somewhat negative image. Therefore, we had to use some different words. We came up with the new word “Locabo” after the English phrase “low-carb” and then it spread throughout Japan.
Locabo is not strict but rather a loose carbohydrate restriction. By definition, the diet tries to keep the carbohydrate intake amount per day to around seventy to one hundred and thirty grams in total, by taking twenty to forty grams per meal, three times a day and also a dessert or sweets up to ten grams.

The difference from a strict carbohydrate restriction is that by eating at least seventy grams of carbohydrates, it avoids an extremely low-carbohydrate condition that results in “Ketosis.”
Also, a strict carbohydrate restriction diet makes food choices very limited, but Locabo has a variety of foods you can enjoy. As long as you keep adjusting carbohydrate intake, you can eat a variety of foods such as meat, fish, cheese, and vegetable dishes without thinking about calories."
[References: Satoru Yamada. The truth of carbohydrate restriction. Gentosha books, Nov. 2015, Page 114]
2. Summary of the effects of “Locabo"
The leading advocate for promoting low-carb diets in Japan is Dr. Satoru Yamada, and summarizing his thoughts, we get the following points:
(1) When blood sugar levels rise due to meals, insulin is secreted from the pancreas. Excessive insulin secretion may potentially lead to weight gain. Japanese individuals have a weaker ability to secrete insulin compared to Westerners, and many people experience blood sugar abnormalities even if they are not overweight. More than half of those who develop typeⅡdiabetes have a BMI less than twenty-five.
(2) The higher the frequency of insulin secretion and the higher the upper limit of blood sugar levels, the greater the burden on the pancreas. Over time, this burden can lead to impaired insulin secretion and the onset of diabetes. Additionally, sharp fluctuations in blood sugar levels may potentially contribute to aging, cell cancerization, cognitive disorders (Alzheimer's), and an increased risk of developing cardiovascular diseases.
(3) The only factor that raises blood sugar levels is carbohydrates. By adopting a low-carb diet, it is possible to moderate the increase in blood sugar levels.
Nutrients such as proteins, fats, and dietary fiber, aside from carbohydrates, have the ability to suppress a rapid rise in blood sugar.
In other words, fried rice can control the rapid increase in blood sugar more effectively than white rice.

(4) The belief that reducing fat intake is essential for health has been unquestionably accepted in Japan for a long time. However, various data from the twenty-first century has revealed that even if one reduces fat consumption, it may not lead to improvements in blood lipid levels or prevent heart disease and obesity.
While trans fats should be avoided, there is no need to unnecessarily restrict other types of fats. As for the intake of animal fat (saturated fat), such as those found in meat, studies indicate that, when limited to the Japanese population, there is no association with the incidence of myocardial infarction or stroke (data from 2013).
(5) Even with reduced carbohydrate intake, the brain can utilize ketones (produced from fatty acids) as an energy source. In cases of extreme carbohydrate restriction, an accumulation of ketones in the body can lead to a shift in blood acidity, potentially causing a condition known as ketoacidosis. Given the associated risks, it is advisable not to engage in extreme carbohydrate restriction.
(6) Very few individuals can sustain strict caloric limits or a low-fat diet over the long term. A more lenient approach to carbohydrate restriction is easier to adhere to since it doesn't require constant caloric monitoring, and it often yields more favorable results compared to other dietary approaches. It is important to broaden the options for individuals, exploring which dietary approach suits them best.
3.The increasing prevalence of diabetes in Japan
According to the National Health and Nutrition Survey, per capita daily intake of carbohydrates has been consistently decreasing for over sixty years. The daily intake of energy, too, increased until the early 1970’s, but has been on a declining trend since then.
Nevertheless, in recent years, the number of diabetics and latent diabetics with abnormal blood sugar levels continues to rise.
For more detailed data on this trend and other factors I can think of other than carbohydrate intake, please refer to the following article.
【Related article】Diabetes is Increasing Despite Decreased Carbohydrate Intake
4. Is controlling insulin the key to weight loss?
In terms of controlling blood sugar levels, I believe a moderately low-carb diet can be effective. However, what about the issue of obesity?
According to Gary Taubes, the author of "Why We Get Fat," the debate over whether "overeating calories" or "carbohydrates" are the cause of weight gain has been ongoing since the early 1800’s. The reason behind this is that with a low-carb diet, individuals were able to lose weight without worrying about the quantity of other calorie sources such as meat and fats.
This contradicted the calorie theory and faced strong opposition from experts who staunchly believed in it and considered fats harmful to the heart[1], but now it is said that recent intervention studies have demonstrated the significant weight loss effects of a low-carb diet[2], solidifying its position in the field.
Experts who advocate for a low-carb diet seem to believe in the carbohydrate-insulin model, suggesting that carbohydrates cause weight gain by raising blood sugar levels and promoting insulin secretion. According to this model, it is deemed acceptable to consume proteins and fats that do not stimulate insulin secretion, as long as carbohydrates are reduced, in order to compensate for calories. However, I find this explanation to be insufficient.

What I would like to add is as follows: a diet leaning towards easily digestible refined carbohydrates and proteins (processed foods) is rapidly digested. As such a diet continues, you feel hungrier, and intestinal starvation is likely to occer.
The characteristics of carbohydrates (dilution effect, push-out effect) further accelerate the occurrence of intestinal starvation.
(In other words, what is related to intestinal starvation are complex carbohydrates such as starch, rice, and flour, not simple carbohydrates like sugar.)
[Related article]
The Dilution Effect/ Pushing Out Effect of Carbohydrates
Therefore, as a countermeasure, we must do the opposite in order to lose weight; not only to reduce carbohydrates to a certain extent but also to increase the intake of foods that take longer to digest (proteins, fats, dairy products, etc.) and foods rich in fiber, so that undigested food will remain abundant in the intestines. (In this regard, the concept of glycemic index [GI] and glycemic load [GL] is very important.)

While advising to consume unlimited amounts of meat and animal fats (saturated fatty acids) doesn't seem accurate, I believe it is important to combine a variety of foods-low-GI carbohydrates, plant-based proteins such as legumes and nuts, unsaturated fatty acids found in fish and plant oils, dairy products, and fibrous vegetables, etc.-to enhance the feeling of fullness.
As a result, the diet may end up resembling a lenient low-carb diet, but my stance is that carbohydrates are not a direct cause of obesity but rather an indirect factor that can induce intestinal starvation. Therefore, I have reservations about strict carbohydrate restrictions such as the ketogenic diet.
Additionally, even if insulin is considered to promote fat storage, I do not believe it is the fundamental cause of obesity.
Some people who advocate a low-carb diet say, "As long as you adjust your insulin secretion, you can eat anything without worrying about calories, even fatty foods, cheese, and meat. And since that's how you lost weight, it was the carbohydrates, not the caloric intake, that was the reason." I don’t think this explanation is correct.
5. The widespread issue of unbalanced and low-quality diets in Japan
In recent years, as the global rise in obesity becomes a significant concern, I believe that for those who tend to gain weight, easily digestible refined carbohydrates are undeniably central factors contributing to weight gain.
However, not everyone gains weight because they eat carbohydrates; factors such as the type of carbohydrates (those with a high GI value), unbalanced diets, and irregular eating habits (such as skipping breakfast or late-night meals) are also associated with the issue.
For instance, focusing solely on caloric and/or carbohydrate "intake," might make it seem like skipping breakfast or opting for simple meals like cup noodles, "snack bread and rice balls," or fast food for lunch is a reasonable choice. It may even appear that not eating vegetables could be somewhat helpful in reducing a few carbs or calories.

However, repeatedly consuming a “low-quality diet” low in fiber and nutrients, rich in carbohydrates, and experiencing recurrent hunger, could potentially increase the risk of developing diabetes and blood sugar abnormalities as well as obesity, don't you think?
While I cannot provide data, to the best of my knowledge, there has been a significant decline in the "quality of meals" among temporary laborers in factories and workplaces, and low-income individuals in Japan in recent years.
When trying to cut down on food expenses, carbohydrates are the cheapest source of calories available, offering a temporary sense of satisfaction.
The bottom line
(1) and (2) are summarized from the contents of "Diabetes is Increasing Despite Decreased Carbohydrate Intake."
(1) The number of diabetes patients in Japan has been steadily increasing since the estimated count began in 1997, rising from 6.9 million to reach 10 million in 2016. Including pre-diabetics with blood sugar abnormalities, the total exceeds 20 million in 2016 (approximately one in six people). Compared to Western populations, Japanese people have a weaker ability to secrete insulin, and over half of those who develop typeⅡdiabetes have a BMI lower than 25.
(2) In Japan, there has been a decreasing trend in caloric and carbohydrate intake for over fifty years. At least in the context of Japan, the rise in obesity, diabetes, and blood sugar abnormalities cannot be solely explained by the amount of caloric and carbohydrate intake alone. Factors such as high glycemic index (GI) foods, sugars, unbalanced diets, and irregular lifestyles including not eating breakfast, may be related to this increase.
(3) Focusing solely on caloric and/or carbohydrate intake might make it seem reasonable to skip breakfast, opt for quick and easy meals like instant noodles or fast food for lunch, and even consider eliminating vegetables.
However, a low-quality diet skewed towards easily digestible carbohydrates and repeated bouts of hunger, may not only increase the risk of developing health issues such as blood sugar abnormalities but also contribute to obesity.
(4) My stance is that the recent increase in (A) the risk of obesity and (B) the prevalence of blood sugar abnormalities is due to the different properties of carbohydrates.
As for (B), the major influence is how a diet containing carbohydrates raises blood glucose levels and its relationship with insulin. In contrast, (A) is associated with easily digestible carbohydrates diluting the food (nutrients) consumed and, under certain conditions, leading to intestinal starvation.
In short, in my theoretical framework, the fundamental issue with obesity is that one’s 'set-point' for body weight goes up through intestinal starvation, and carbohydrates indirectly affect that.
(5) Reducing carbohydrate intake is not the only important factor in decreasing the risk of obesity and blood sugar abnormalities. It is also important to consume low-GI grains, incorporate foods from other food groups (such as meat, fish, vegetables, nuts, dairy, seaweed, etc.) in the diet, and maintain a regular eating schedule (e.g. three meals a day).
All of these practices contribute to slowing down digestion, moderating the speed of absorption, and helping to keep blood glucose levels stable. The concepts of "second meal effect" and "resistant starch" are also important in this regard.
In terms of weight loss, it is crucial to have undigested food consistently remaining in the intestines by consuming more foods that take longer to digest (e.g. proteins, fats) and more fibrous foods.
This approach helps reduce the sensation of hunger, leading to a gradual decrease in absorption rates. Therefore, controlling hunger is, in fact, the key for achieving successful weight loss, in my opinion.
(6) I believe that simple carbohydrates like sugar are significantly related to blood sugar abnormalities. However, the cause of inducing intestinal starvation lies in complex carbohydrates (polysaccharides) such as starch and wheat flour, and not in simple sugars.
<References>
[1] Gary Taubes. Why We Get Fat. New York: Anchor books, 2011, Pages 159-160.
[2] Jason Fung. The Obesity Code. Greystone books, 2016, Page 100.
- 1 / 8
- »